






CNC machining is a precise manufacturing process vital for creating medical device prototypes. It enables developers to produce components with tight tolerances using biocompatible materials like titanium, stainless steel, and PEEK. These prototypes are critical for validating designs, ensuring compliance with Australia's stringent Therapeutic Goods Administration (TGA) standards, and preparing for market entry.
| Method | Precision | Speed | Material Options | Cost per Part (AUD) | Best Use Case |
|---|---|---|---|---|---|
| CNC Machining | ±0.01–0.05 mm | 1–5 days | Production materials | $50–$500+ | Functional testing, final validation |
| 3D Printing | ±0.1–0.3 mm | Hours–1 day | Limited medical grades | $5–$100 | Concept models, complex geometries |
| Injection Moulding | ±0.02–0.1 mm | 2–8 weeks | Wide polymer selection | $1–$10 (high volume) | High-volume production |
| Vacuum Casting | ±0.1–0.2 mm | 2–5 days | Polyurethane variants | $20–$150 | Bridge production, small batches |
CNC machining stands out for its ability to produce high-fidelity prototypes with production-grade materials, ensuring safety, functionality, and compliance with Australian regulations.
The process begins with creating detailed 3D models using CAD software. These models define the dimensions, tolerances, and surface finishes required for the prototype. For medical prototypes, the designs must also account for biocompatibility and sterilisation requirements. The CAD files act as blueprints, guiding the CNC machine's cutting paths and tool selection.
Material selection happens alongside design refinement. Popular choices for medical applications include biocompatible metals like titanium alloys and stainless steel 316L, which are commonly used for implants and surgical tools. Medical-grade plastics such as PEEK (polyetheretherketone) and PMMA (polymethyl methacrylate) are also widely used due to their chemical resistance and ability to endure multiple sterilisation cycles. The material must align with the chosen sterilisation method, such as steam autoclaving, gamma radiation, or ethylene oxide gas.
Engineers also need to consider the prototype's specific purpose. For instance, a surgical guide will have different material demands compared to the housing of a diagnostic device. Factors like mechanical strength, wear resistance, and compatibility with human tissue or bodily fluids are carefully evaluated. These decisions shape the subsequent machining and finishing stages.
Once the design and material are finalised, the process moves on to machining and post-processing, where precision and quality take centre stage.
Precision machining is at the heart of producing medical prototypes that meet Australia's rigorous standards. The machining process typically involves roughing to remove excess material, followed by finishing to achieve the exact dimensions required for components like orthopaedic implants.
Quality control is a continuous process, with tools like coordinate measuring machines (CMMs) and optical systems verifying dimensions against the CAD model. Any deviations are corrected immediately, avoiding costly rework and ensuring compliance with medical device standards.
Post-processing plays a vital role in determining the prototype's performance. Surface treatments such as painting, powder coating, or silkscreening are often applied to create smooth, bacteria-resistant finishes. These treatments not only enhance patient comfort but also improve the appearance of patient-facing devices.
Sterilisation compatibility is another key focus during post-processing. Materials must withstand exposure to harsh chemicals, high-temperature steam (121°C to 134°C), or gamma radiation without compromising their properties. Testing during this stage ensures the prototype can endure sterilisation processes while maintaining its integrity.
A final inspection checks dimensions, surface quality, and material certifications. This thorough approach ensures the prototype meets the stringent standards required for medical device development and regulatory approval in Australia.
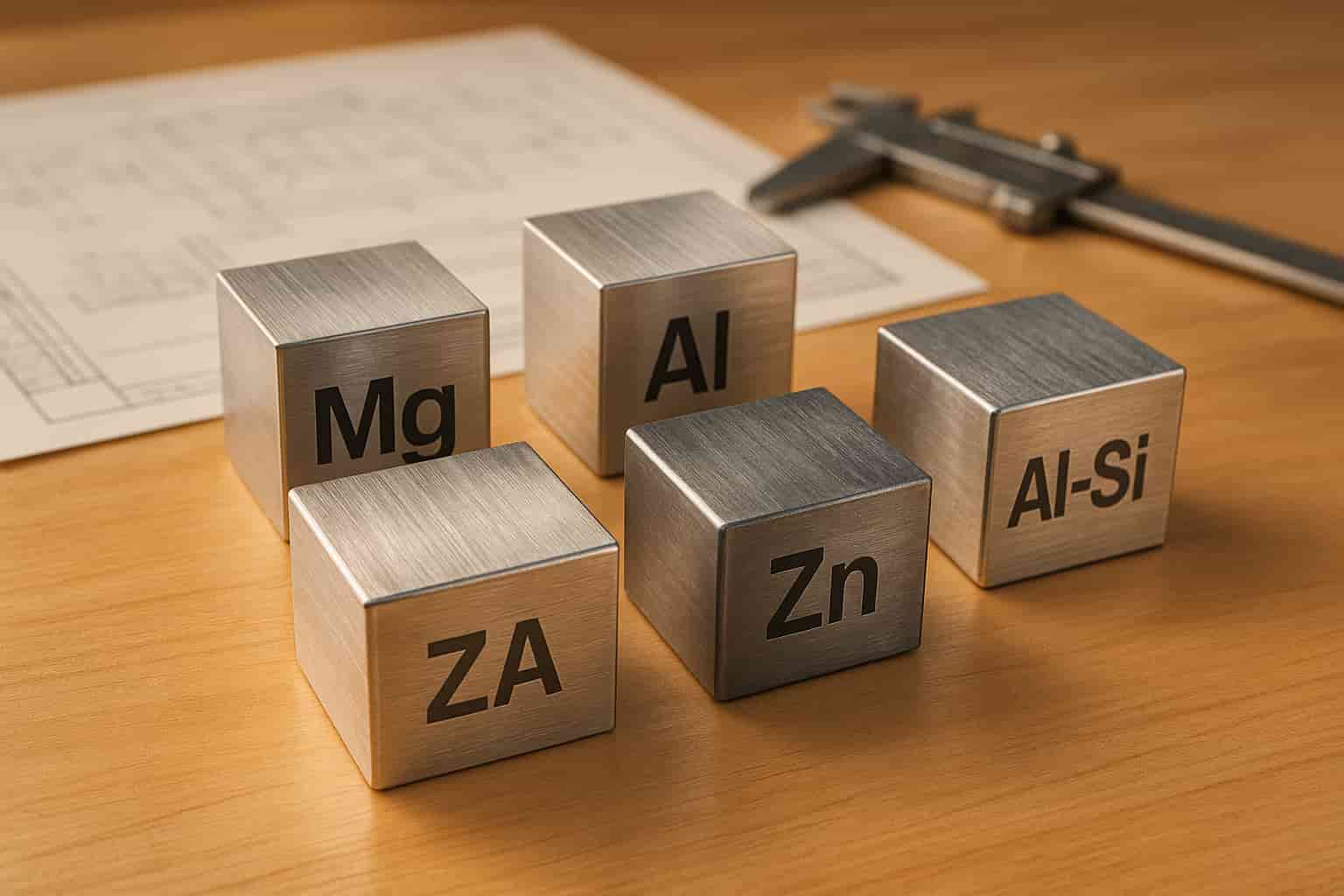
Choosing the right material for medical device prototypes involves balancing biocompatibility, mechanical performance, and manufacturability. The material selection process significantly affects how well the prototype performs, the time it takes to secure regulatory approval, and the product's overall success in the market. These considerations guide the use of specific materials, starting with titanium alloys for demanding implant applications.
Titanium alloys, particularly Ti-6Al-4V, are a go-to choice for implantable device prototypes. Their excellent biocompatibility and resistance to corrosion make them ideal for load-bearing applications like hip replacements and dental implants. Titanium's ability to bond with bone (osseointegration) makes it indispensable in orthopaedics. However, its high cost and machining difficulties require careful consideration during the prototyping phase.
Stainless steel 316L is widely used for surgical instruments and temporary implants. It offers strong corrosion resistance in bodily fluids and is easier to machine compared to titanium. This makes it suitable for creating complex geometries during prototyping. However, its magnetic properties can limit its use in devices that need to be MRI-compatible.
Medical-grade polymers provide flexibility for non-implantable devices and housings. PEEK (polyetheretherketone) is particularly valued for its chemical inertness, durability under repeated sterilisation, radiolucency (important for imaging), and wear resistance.
PMMA (polymethyl methacrylate) is a preferred material for optical applications and temporary implants, such as bone cement. Its transparency and ease of sterilisation make it a good fit for diagnostic equipment housings and fluid-handling components. However, its brittleness restricts its use in high-stress environments.
For less critical components, cost-effective plastics like ABS and polycarbonate are practical options. These materials are commonly used for electronics housings and non-critical components. They offer good impact resistance and can be sterilised using gamma radiation or ethylene oxide, making them ideal for single-use devices and protective housings.
Understanding the properties of each material is essential for making informed decisions during prototype development. Each material has unique strengths and limitations that must align with the device's purpose and regulatory requirements. Here's a quick comparison of the key properties and applications for common materials:
| Material | Biocompatibility | Machinability | Cost | Sterilisation Methods | Common Applications |
|---|---|---|---|---|---|
| Titanium Ti-6Al-4V | Excellent | Challenging | High | Steam, gamma, EtO | Implants, surgical tools |
| Stainless Steel 316L | Excellent | Good | Low | Steam, gamma, EtO | Surgical instruments |
| PEEK | Excellent | Moderate | Moderate–High | Steam, gamma, EtO | Spinal implants, imaging |
| PMMA | Good | Excellent | Low–Moderate | Gamma, EtO | Bone cement, optics |
| Medical ABS | Good | Excellent | Low | Gamma, EtO | Housings, disposables |
| Polycarbonate | Good | Good | Moderate | Gamma, EtO | Protective covers, lenses |
Relative costs play a major role in material selection. For example, titanium's high price often makes it impractical for early-stage prototypes, where more affordable and easier-to-machine alternatives are preferred. Titanium is typically reserved for final validation prototypes that closely replicate the commercial product.
Machinability is another critical factor, as it directly affects manufacturing timelines and costs. Materials that are harder to machine often require specialised tools and slower cutting speeds, which can increase production times compared to more easily machined options.
Sterilisation compatibility is equally important. Materials must endure processes like steam autoclaving, gamma radiation, or ethylene oxide sterilisation without degrading. For instance, steam sterilisation is a cost-effective method but demands materials that can withstand high heat and humidity. Gamma radiation, on the other hand, is better suited for heat-sensitive materials, though repeated exposure can weaken certain polymers.
In the early stages of development, engineers often use easily machined materials to test and refine design concepts. Once the design is validated, the focus shifts to using the final materials for regulatory testing. This phased approach helps control costs while ensuring the final prototype meets performance expectations.
In Australia, regulatory compliance requires thorough documentation of material certifications and traceability. Each material batch must include certificates verifying compliance with relevant ISO standards, such as ISO 10993 for the biological evaluation of medical devices. This documentation is essential for navigating the regulatory approval process smoothly.
CNC machining stands out for its precision in medical device prototyping, achieving tolerances as tight as ±0.01 mm. This level of accuracy is essential for functional components where even the smallest dimensional changes can impact performance or patient safety.
Another major advantage is the superior surface finish, which often eliminates the need for extensive post-processing. This is particularly beneficial for medical devices that require smooth surfaces to maintain sterility and ensure proper sealing. Additionally, CNC machining allows engineers to work with final production materials, enabling them to test prototypes under conditions that closely mirror the final product.
Scalability is another strength. Once a CNC program is validated, it can seamlessly transition from prototyping to medium-volume production. This ensures consistency between prototype testing and initial production runs while reducing the risk of unforeseen issues during scaling.
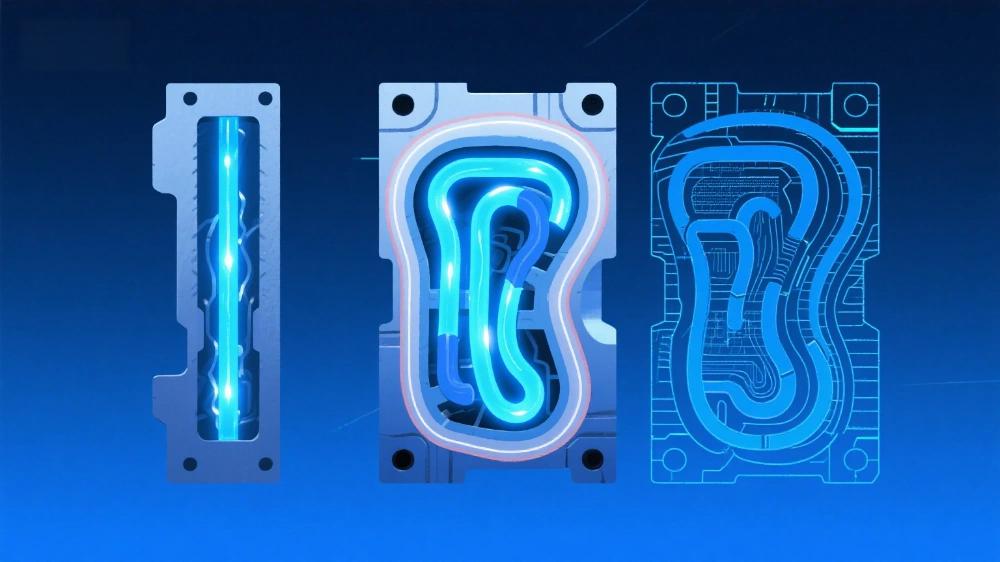
However, CNC machining does come with challenges. High setup costs can make it less practical during the early stages of design when multiple concepts are being explored. The process also requires skilled operators and specialised tools, which can increase costs further. Additionally, certain designs - like those with internal channels or undercuts - may be unachievable, limiting flexibility compared to additive manufacturing. For intricate parts, longer lead times can also slow development, as design changes often necessitate new tooling or programming updates.
Here’s a comparison of CNC machining with other prototyping methods based on key factors such as precision, speed, material options, cost, and their best use cases for medical devices:
| Method | Precision | Speed | Material Options | Cost per Part (AUD) | Best Use Case |
|---|---|---|---|---|---|
| CNC Machining | ±0.01–0.05 mm | 1–5 days | Production materials | $50–$500+ | Functional testing, final validation |
| 3D Printing | ±0.1–0.3 mm | Hours to 1 day | Limited medical grades | $5–$100 | Concept models, complex geometries |
| Injection Moulding | ±0.02–0.1 mm | 2–8 weeks (setup) | Wide polymer selection | $1–$10 (high volume) | High-volume production |
| Vacuum Casting | ±0.1–0.2 mm | 2–5 days | Polyurethane variants | $20–$150 | Bridge production, small batches |
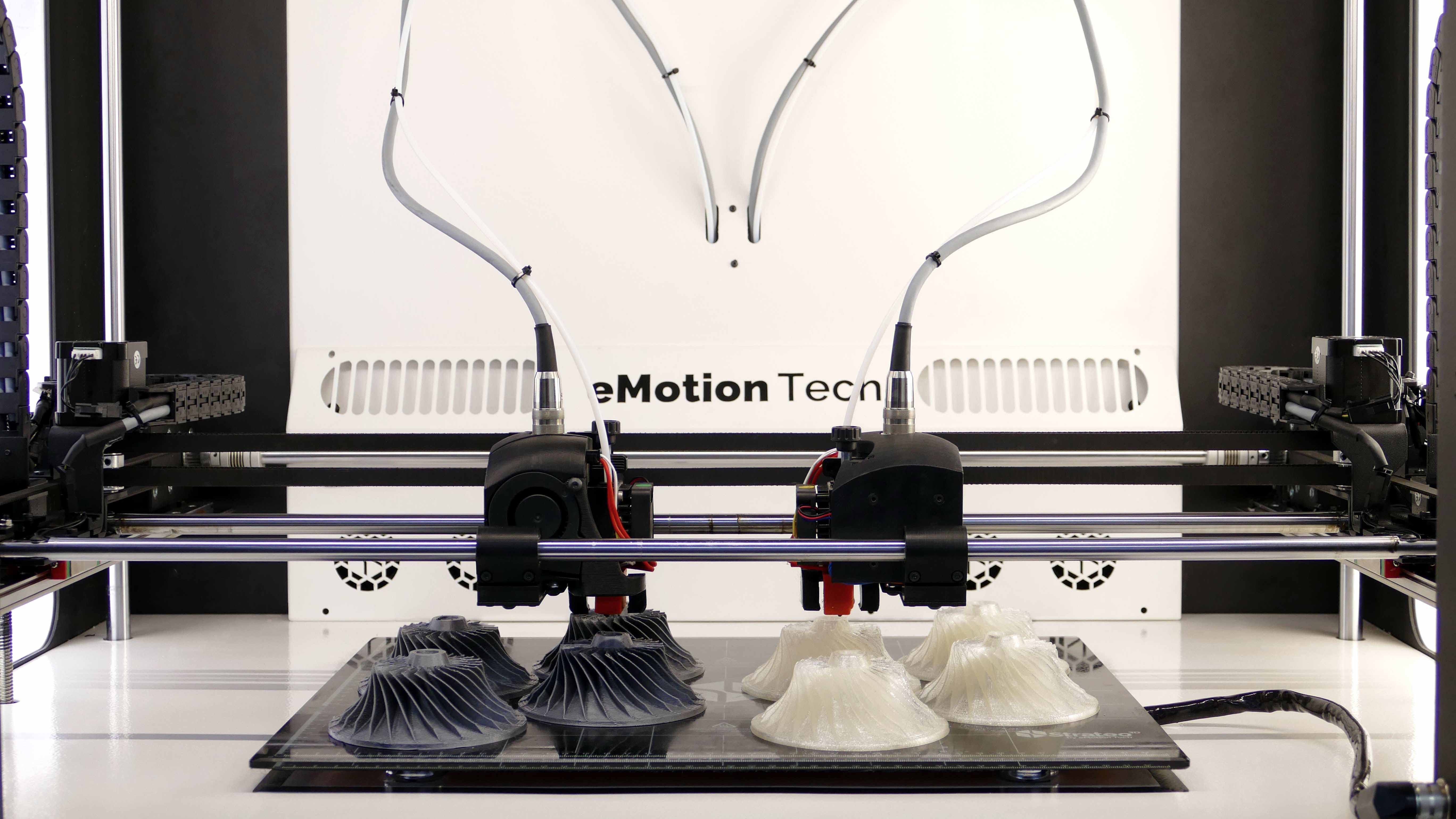
3D printing is ideal during the initial design phase, offering rapid iteration and the ability to create complex internal geometries. However, its layer-by-layer approach often results in surface textures that may need additional finishing, especially for medical applications.
Injection moulding, on the other hand, becomes cost-effective for high-volume production. While the initial tooling investment - ranging between $10,000 and $100,000 AUD - makes it unsuitable for prototyping, it provides excellent repeatability and access to a wide range of medical-grade polymers.
Vacuum casting serves as a bridge between prototyping and low-volume production. It’s particularly useful for creating functional prototypes using polyurethane materials that closely mimic production plastics. Silicone moulds in this process can typically produce 15–25 parts before requiring replacement, making it ideal for small batch testing or early market validation.
The choice of prototyping method depends largely on the stage of development. Early concept validation often benefits from the speed and flexibility of 3D printing, while functional testing requires CNC machining for its precision and material accuracy. Pre-production validation may rely on vacuum casting to test market response before committing to the higher tooling costs of injection moulding.
Cost considerations go beyond the per-part price. While 3D printing offers lower individual part costs, its material limitations may necessitate additional validation. Conversely, CNC machining’s higher per-part cost is justified by its ability to test with final production materials, ultimately reducing overall development time and risks.
In Australia, regulatory requirements also influence the choice of prototyping method. For Therapeutic Goods Administration (TGA) submissions, demonstrating material traceability and process validation is critical. CNC machining, with its established processes and certified materials, often provides a clearer regulatory pathway compared to some additive manufacturing methods. These trade-offs are crucial when aligning prototyping approaches with Australia’s stringent regulatory and quality standards.
In Australia, the Therapeutic Goods Administration (TGA) serves as the primary regulatory authority for medical devices, shaping key decisions during the prototyping phase. Addressing regulatory requirements early in the development process can help avoid costly redesigns and shorten the time-to-market.
Medical devices are classified by risk level, with lower-risk devices (like Class I) requiring less documentation, while higher-risk devices demand rigorous testing and detailed records. For CNC machined prototypes, the device's classification influences material choices, testing protocols, and the level of process documentation needed.
Biocompatibility is a critical requirement under ISO 10993 standards, which mandate evaluation and testing for materials that will contact the human body. Materials like medical-grade stainless steel 316L, titanium Ti-6Al-4V, and PEEK polymers are commonly used due to their proven biocompatibility and established testing records.
Additionally, the inclusion process for the Australian Register of Therapeutic Goods (ARTG) requires detailed manufacturing information. CNC machining is particularly advantageous here because of its precise and repeatable process parameters, which support compliance efforts.
To enhance risk management, integrating ISO 14971 principles into the prototyping phase is essential. This involves assessing material, surface, and dimensional risks to ensure patient safety. These regulatory demands naturally extend to robust quality control and traceability systems.
Once regulatory documentation is in place, stringent quality control measures ensure safety and compliance. Every raw material must be traceable back to its source, supported by certificates for heat treatment, chemical composition, and biocompatibility. Maintaining this traceability throughout prototyping and production is non-negotiable.
Medical device prototypes often have demanding dimensional accuracy requirements. For critical components, tolerances as tight as ±0.025 mm - or even finer - may be necessary, especially for parts designed to interface with other devices or the human body. CNC machining is well-suited to achieve such precision, but it requires rigorous measurement protocols using tools like coordinate measuring machines (CMMs) and optical measurement systems.
Surface finish is another vital consideration. Many medical applications demand surface roughness (Ra) values below 0.8 micrometres to ensure biocompatibility and enable effective cleaning. While CNC machining can achieve these finishes, thorough documentation - including profilometer measurements - is essential.
Establishing controlled processes during prototyping simplifies later validation. For some applications, environmental factors like temperature and humidity during machining may also need monitoring.
Compliance with ISO 13485 standards is crucial for medical device manufacturing. This involves systematic documentation of design files, material certificates, inspection reports, and process parameters. Such records not only ensure compliance but also streamline the transition from prototyping to production.
Cleaning and sterilisation are critical considerations during both design and manufacturing. Factors like surface finish, material selection, and geometric design influence how easily a device can be cleaned and sterilised. Prototypes should be designed to facilitate these processes.
When prototype modifications are necessary, change control procedures must be followed. Any adjustments to materials, dimensions, or processes should be documented and evaluated for their potential impact on safety and performance. Implementing a structured approach to change management during prototyping helps pave the way for a smoother production phase.
The precision and consistency of CNC machining make it an ideal choice for meeting the strict quality and regulatory standards required for medical devices in Australia. This approach ensures that prototypes are not only compliant but also ready for the demands of the local market.
Australia's medical device industry operates in a challenging environment, juggling strict regulations and the need for rapid innovation. Partnering with an all-in-one manufacturing provider simplifies the prototyping process by bringing together services like CNC machining, 3D printing, vacuum casting, and assembly under one roof. This integrated approach not only minimises delays but ensures consistent quality and keeps accountability in one place.
The financial benefits go beyond just bulk discounts. Integrated manufacturers can cut costs by optimising material use across processes, grouping similar tasks to save on setup expenses, and avoiding the extra mark-ups that come with working through multiple suppliers. For Australian medical device companies with limited budgets, these savings can be the deciding factor in whether a promising idea moves forward or gets shelved due to high costs.
Another key advantage is the ability to run parallel processes. For example, while one team works on machining critical components, another can prepare tooling for secondary tasks or start planning the assembly. This simultaneous workflow can significantly cut down prototyping timelines compared to the traditional, multi-vendor approach.
Additionally, this streamlined process supports compliance with TGA requirements and ISO 13485 standards. By consolidating operations, manufacturers can provide the detailed documentation needed for regulatory submissions, setting the foundation for product success.
Mastars builds on these advantages with a fully integrated service model designed to meet the specific needs of Australia's medical device sector. Their rapid CNC machining services are ideal for the iterative nature of medical device development, where designs often evolve based on clinical feedback.
For early-stage validation, their 3D printing services provide a cost-effective way to visualise concepts. Developers can use printed prototypes to refine form and fit before moving on to CNC-machined versions for functional testing and regulatory approval.
When it comes to producing small runs of complex, biocompatible parts, Mastars' vacuum casting services shine. Using a single master pattern, they can efficiently create limited prototypes suited for clinical trials and user testing.
Mastars also handles assembly in-house, making them a one-stop shop for complex medical devices. Their expertise in precise assembly and contamination control is particularly valuable for devices that combine electronic and mechanical components.
Leveraging Industry 4.0 technologies, Mastars supports the detailed documentation required for TGA submissions and ISO 13485 compliance. Automated quality checks and digital process monitoring reduce the need for manual documentation while ensuring full traceability.
Cost efficiency is a priority for Australian startups and smaller developers, and Mastars' integrated approach eliminates many hidden expenses. By avoiding inter-facility shipping, duplicate setup fees, and coordination challenges, they help keep projects on budget. Their custom quoting system further ensures transparency, giving clients a clear understanding of costs upfront.
With precise CNC machining and strict material standards, Mastars meets both design and regulatory requirements. Their fast turnaround times align perfectly with the accelerated pace of medical device development, helping companies maintain momentum and seize market opportunities.
CNC machining plays a crucial role in medical device prototyping, turning innovative ideas into products that meet both market demands and stringent regulatory standards. This guide has highlighted how this manufacturing technique provides the precision and material compatibility needed to develop reliable medical devices.
A structured workflow is vital for success - starting with precise designs and selecting biocompatible materials, followed by machining and post-processing. This step-by-step approach ensures each prototype iteration moves closer to the final product while meeting the strict requirements of healthcare applications.
Biocompatible materials like medical-grade stainless steel, titanium alloys, and PEEK plastics are the backbone of safe and effective devices. Knowing the specific properties of these materials - such as their resistance to corrosion and compatibility with sterilisation methods - is essential for achieving both high performance and regulatory approval.
In Australia, adherence to TGA guidelines and ISO 13485 standards influences every stage of prototyping. Incorporating quality control and traceability from the outset - not as an afterthought - is critical for success in this highly regulated industry.
When it comes to achieving precise finishes, accurate dimensions, and material properties that closely resemble production parts, CNC machining stands out. While 3D printing is excellent for validating initial concepts, CNC machining provides the precision and durability required for functional testing and clinical trials.
As previously mentioned, working with integrated manufacturing partners simplifies the entire process. Companies like Mastars not only deliver rapid CNC machining but also offer complementary services such as 3D printing, vacuum casting, and assembly. This integrated approach reduces coordination challenges, ensures quality, and keeps hidden costs in check, creating a seamless transition from prototype to production.
For Australian developers, the challenge lies in balancing innovation, compliance, speed, and cost. CNC machining, supported by experienced partners like Mastars, ensures the precision and compliance needed to prioritise patient safety while meeting these demands effectively.
CNC machining is known for its accuracy, consistency, and ability to handle a diverse range of strong, durable materials. These qualities make it an excellent choice for producing intricate and functional medical device prototypes that closely resemble the final product in both form and function.
While 3D printing is often preferred for quick and budget-friendly prototypes, CNC machining offers superior surface finishes and is well-suited for scaling up to larger production runs. On the other hand, injection moulding may be more economical for mass production, but CNC machining shines in smaller runs or when precision, fine details, and material performance are essential - requirements often found in medical applications.
When creating CNC machined medical prototypes in Australia, material selection is a critical step governed by the Australian Regulatory Guidelines for Medical Devices (ARGMD). The materials must be biocompatible, capable of withstanding sterilisation processes, and adhere to strict safety standards.
Additionally, the chosen materials must meet classification and conformity assessment criteria, ensuring they align with the Essential Principles for safety and performance. This guarantees that the prototypes are not only safe for medical applications but also fully compliant with Australian regulatory requirements.
Post-processing plays a key role in ensuring CNC machined medical prototypes meet the high-quality and sterilisation standards demanded by the medical industry. It includes steps like polishing, deburring, and applying surface treatments to create smooth, contamination-free finishes.
These processes are essential for minimising microbial retention and ensuring the prototypes can withstand sterilisation techniques such as autoclaving or chemical treatments. By refining surface quality and adhering to strict medical regulations, post-processing ensures that the prototypes are safe, durable, and reliable for use in healthcare settings.