







Medical devices demand uncompromising quality, repeatability, and regulatory compliance. Plastic tooling—the molds, fixtures, and processes that shape polymer components—is the critical enabler of these outcomes at scale. This guide focuses on how to design, validate, and run medical?grade plastic tooling that meets stringent standards while controlling cost and lead time.
Why Plastic Tooling Matters in Medical Devices
Patient safety and biocompatibility: Devices and packaging must be made from materials proven safe for human contact and compliant with ISO 10993 biocompatibility requirements where applicable.
Regulatory rigor: Tooling decisions directly affect validation, inspection, and audit outcomes (e.g., FDA 21 CFR Part 820, ISO 13485).
Precision and consistency: Tight tolerances, clean surfaces, and defect?free parts are non?negotiable for syringes, IV components, diagnostic housings, and surgical instruments.
Scalability and cost control: High?volume disposables and reusable instruments require different tooling strategies to balance upfront investment with lifecycle cost.
Sterilization and cleaning: Materials and finishes must withstand repeated cleaning/sterilization (e.g., EtO, gamma, autoclave) without degradation or loss of dimensional control.
Core Medical Applications and Typical Tooling Choices
These applications illustrate how material selection, process choice, and tooling architecture align with clinical performance, manufacturability, and regulatory expectations.
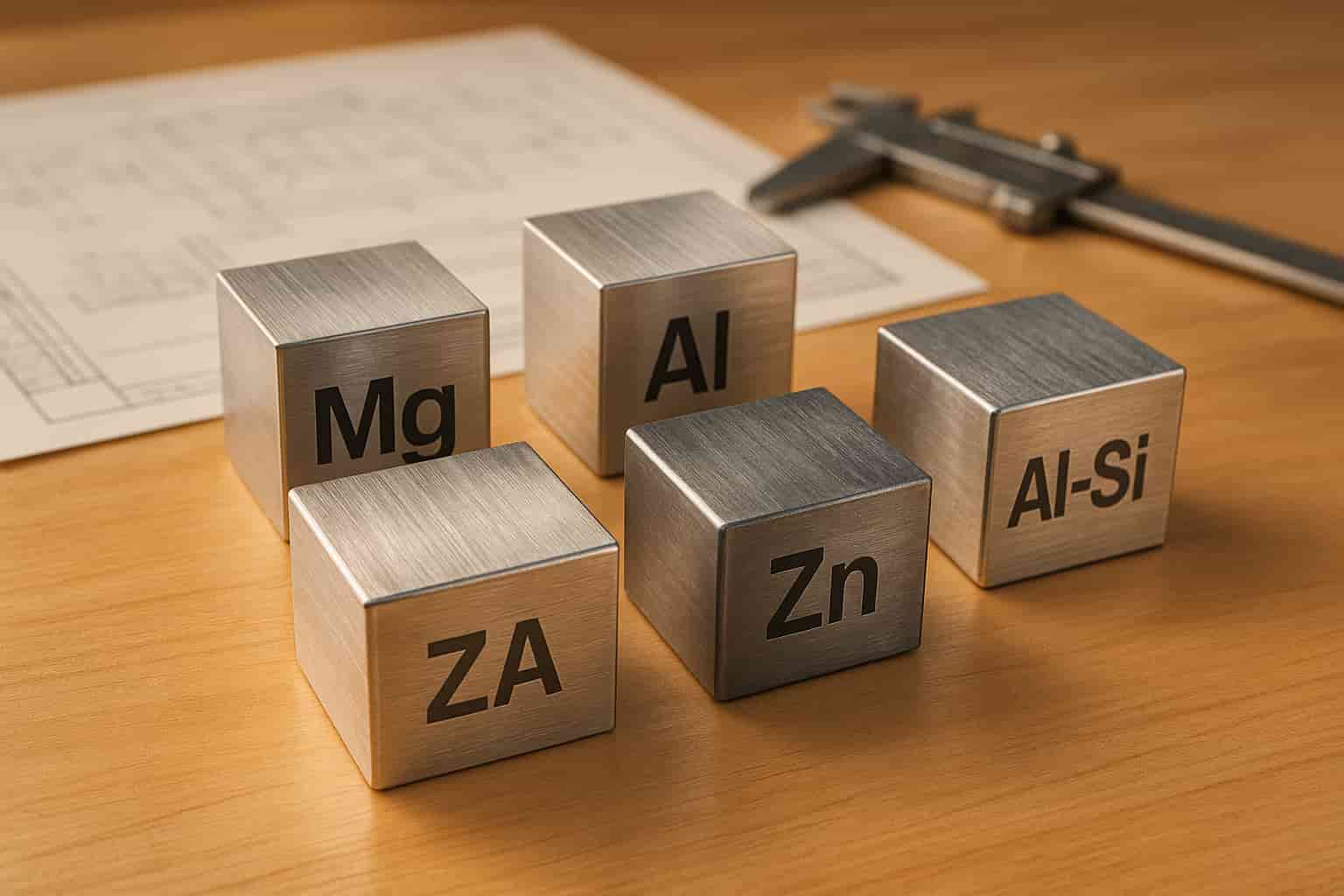
Material and Tool Steel Selection for Medical Tooling
Corrosion?resistant mold steels are essential when molding aggressive chemistries (e.g., PVC), repeated cleaning agents, or when high polish and long life are required. Common grades include S136H and NAR?80 for medical tooling, offering excellent corrosion resistance and high polishability.
Prehardened steels (e.g., P20 variants) are used for many general?purpose medical components where corrosion is not a primary concern, balancing machinability and dimensional stability.
High?hardness hot work steels (e.g., H13) are selected for cores, slides, and wear?prone areas needing toughness and thermal fatigue resistance.
Surface finishes and coatings: For transparent parts (e.g., syringes, optical housings), SPI finishes and optical polishing are common. For textured or grained parts, consider wear?resistant textures and appropriate mold base materials.
ESR (Electroslag Remelting) and high?purity melt practices improve cleanliness and homogeneity—important for large parts and high?cavitation tools where macro?segregation can impact polish, wear, and dimensional control.
PVC considerations: Due to its corrosive off?gassing and high flow, medical PVC tooling often uses corrosion?resistant steels, precise thermal control, and optimized venting to prevent gas traps and surface defects
.Design for Manufacturability and Validation Workflow
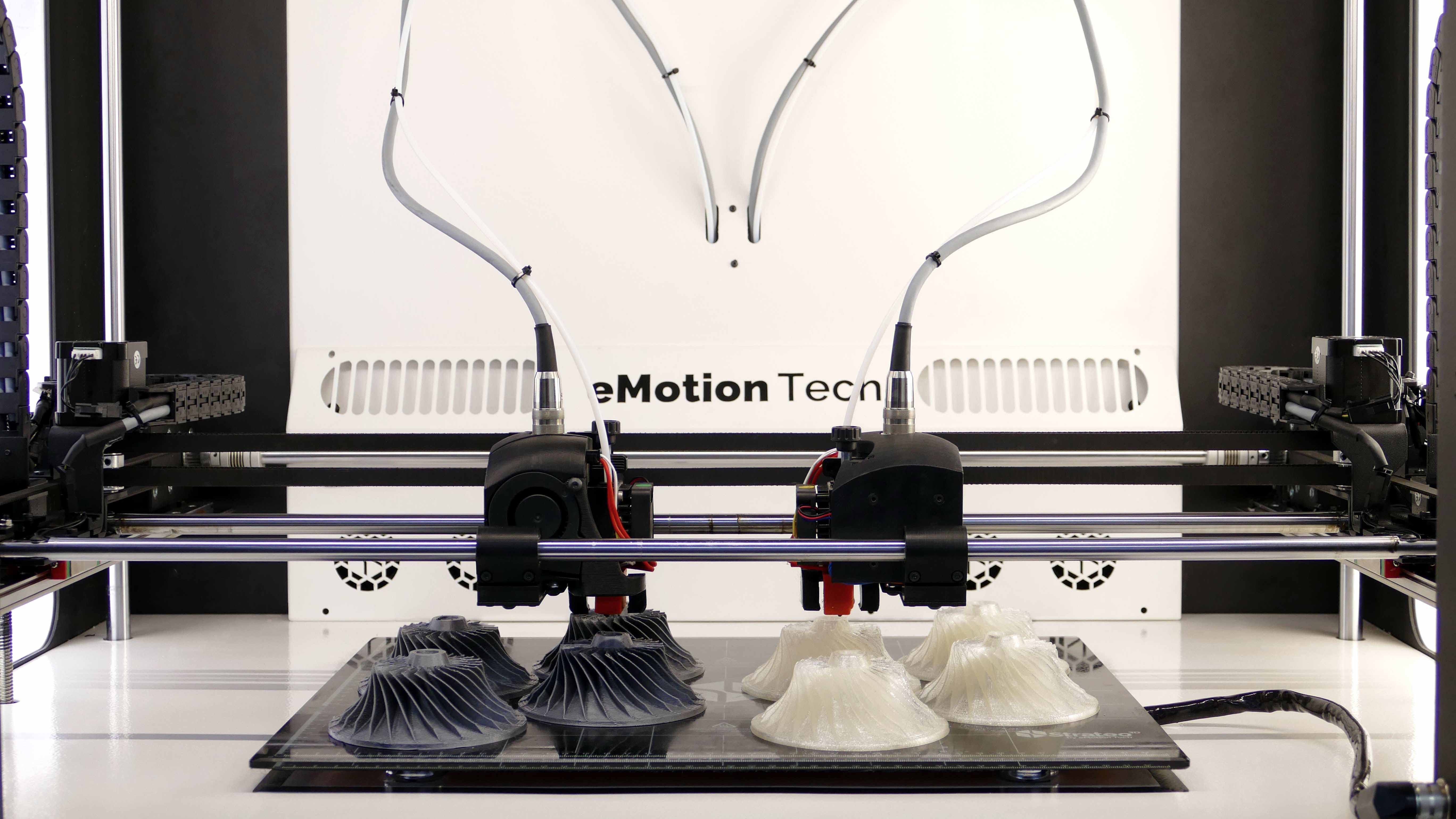
DFM and prototyping: Early engagement with tooling and molding engineers; use CNC/3D?printed prototypes to validate fit, function, and cleanability before steel is cut.
Mold flow analysis: Simulate filling, packing, cooling, and warpage; optimize gate location, runner balance, and cooling layout to reduce short shots, weld lines, and sink marks.
Cleanroom molding: For sterile or cleanroom?packaged parts, design for gowning, material handling, and part demolding that minimizes contamination risk.
Gate and vent strategy: Use pinpoint or fan gates for cosmetics; add micro?vents at weld lines and thick sections; balance runner lengths in multi?cavity tools.
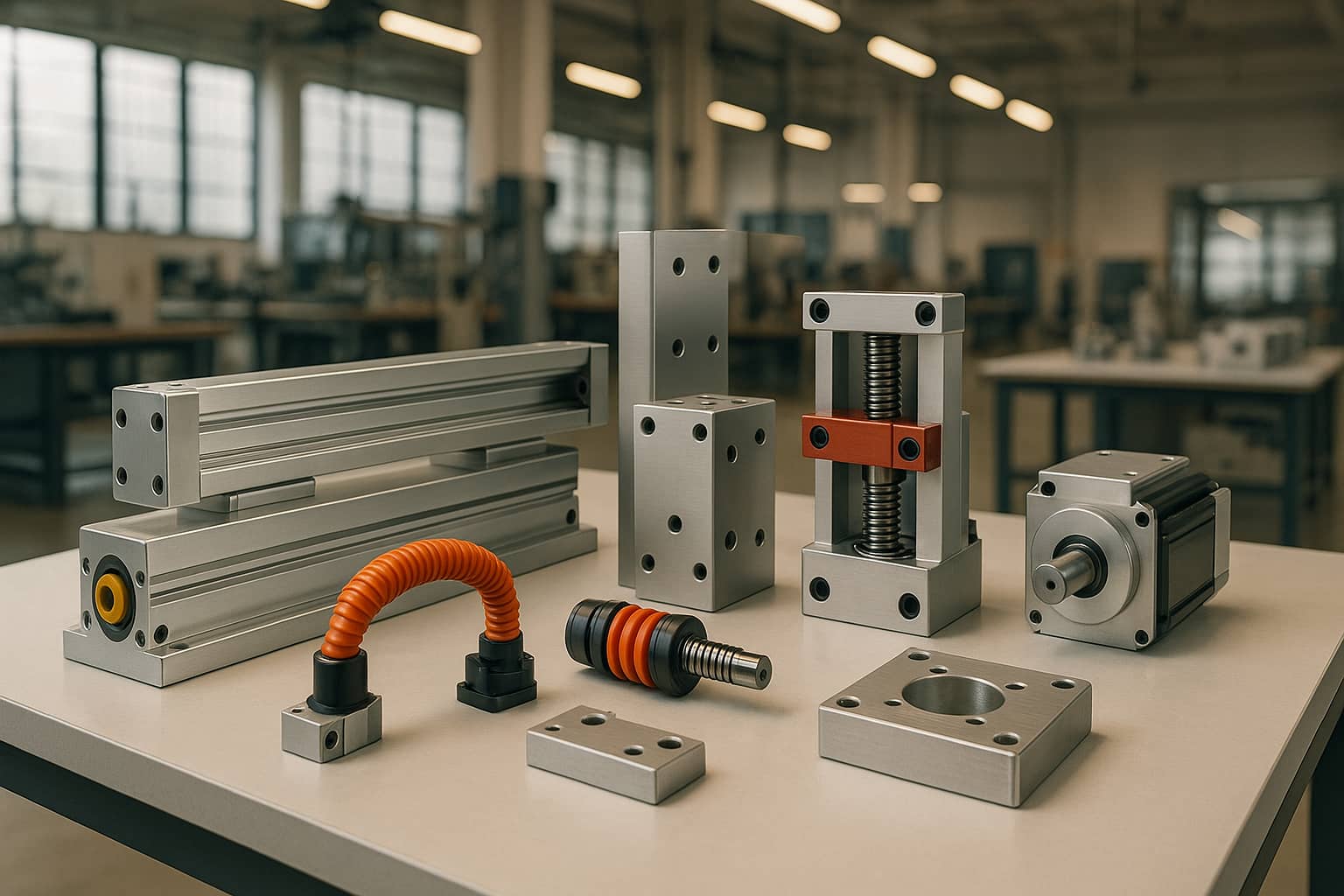
Ejection and automation: Choose ejector pins, sleeves, or stripper plates that ensure damage?free removal; plan for vision/leak testing and automated part handling where required.
First article and validation: Execute T0/T1 sampling, dimensional reports, and capability studies (Cpk); align on sampling plans, gage R&R, and material traceability.
IQ/OQ/PQ and process validation: For equipment and processes impacting patient safety, follow a documented protocol that includes installation qualification, operational qualification, and performance qualification.
Change control and ECOs: Treat design and process changes with the same rigor as initial validation; update risk assessments and re?qualify as needed.
Process Control, Monitoring, and Quality Assurance
In?mold sensing for closed?loop control: Integrating cavity pressure and temperature sensors enables early detection of deviations (e.g., short shots, flash, incorrect dimensions) and supports first?article qualification, root?cause analysis, and cycle optimization. High?resolution sensors (up to 2,500 bar cavity pressure) and non?contact options help maintain part quality in high?precision medical components.
Traceability and data integrity: Automated process monitoring records critical process parameters, supporting 100% part quality control (where applicable), OEE improvement, and regulatory audits.
Cleanliness and contamination control: Design parting lines, shutoffs, and venting to minimize parting line witness and prevent mold sweat; select materials and finishes compatible with validated cleaning/sterilization cycles
.Cost Drivers, Risk Mitigation, and Supplier Selection
Cost drivers:
Cavitation and complexity (multi?cavity, hot runners, side actions/lifters)
Material selection (corrosion resistance, high polish, specialty grades)
Tolerances and surface finish (optical clarity, grained textures)
Validation scope (IQ/OQ/PQ, biocompatibility, sterilization validation)
Regulatory burden (audits, documentation, change control)
Risk mitigation:
Use corrosion?resistant tool steels for aggressive resins (e.g., PVC) and high?cleanliness processes.
Apply conformal cooling and balanced runner/gating to reduce cycle time and improve consistency.
Plan for automation early to reduce human variability and contamination risk.
Freeze critical dimensions and process windows before validation to minimize re?qualification.
Supplier selection criteria:
Proven experience in medical device molding and tooling (ISO 13485 preferred)
In?house design, machining (CNC/EDM), polishing, and tryout
Cleanroom molding and validation support
Strong metrology, documentation, and change?control systems
Transparent DFM feedback and realistic lead times/cost breakdowns
Case Example: Disposable Syringe Barrel
Material: Medical?grade PP for clarity, strength, and regulatory acceptance.
Tooling: 16?cavity cold runner with pinpoint gates at the flange; balanced runner and micro?vents at the end of flow paths; highly polished cavities/cores for transparency; automated part ejection into clean, nestable trays.
Process control: Cavity pressure monitoring to detect fill variation; vision inspection for flash and dimensional outliers; validated EtO sterilization cycle with material compatibility data.
Validation: IQ/OQ/PQ per internal SOPs; sampling plans aligned with device risk class; full lot traceability from resin lot to finished syringe.
Future?Proofing Medical Tooling
Additive manufacturing for inserts and conformal cooling: Faster iteration, complex internal channels, and localized thermal management for reduced cycle time and improved part quality.
Smart molds: Embedding sensors for real?time pressure, temperature, and wear data to enable predictive maintenance and process optimization.
Sustainable materials: Bio?based and recycled resins with verified biocompatibility and sterilization compatibility.
Advanced metrology and digital twins: Inline metrology and simulation?driven DFM reduce rework and accelerate time?to?market.
Conclusion
Medical device plastic tooling is a convergence of materials science, precision engineering, and regulatory discipline. By selecting the right materials (e.g., S136H/NAR?80 for corrosive or high?polish applications), applying rigorous DFM and validation workflows, and leveraging in?mold monitoring for process control, medical device manufacturers can achieve the quality, consistency, and scalability required for life?critical applications.
Glossary
SPI finish: Mold surface finish standard used to specify polishing levels.
EtO: Ethylene oxide sterilization, common for heat?sensitive medical devices.
IQ/OQ/PQ: Installation, Operational, and Performance Qualification protocols for process validation.
Cpk: Process capability index measuring how well a process meets specification limits.
ESR: Electroslag Remelting, a steel?refining process that improves cleanliness and homogeneity.